Abstract
Background
Our experience in trauma center management increased over time and improved with development of better logistics, optimization of structural and technical resources. In addition recent Government policy in safety regulations for road traffic accident (RTA) prevention, such compulsory helmet use (2000) and seatbelt restraint (2003) were issued with aim of decreasing mortality rate for trauma.
Introduction
The evaluation of their influence on mortality during the last 15 years can lead to further improvements.
Methods
In our level I trauma center, 60,247 trauma admissions have been recorded between 1996 and 2010, with 2183 deaths (overall mortality 3.6 %). A total of 2,935 trauma patients with ISS >16 have been admitted to Trauma ICU and recorded in a prospectively collected database (1996–2010). Blunt trauma occurred in 97.1 % of the cases, whilst only 2.5 % were penetrating. A retrospective review of the outcomes was carried out, including mortality, cause of death, morbidity and length of stay (LOS) in the intensive care unit (ICU), with stratification of the outcome changes through the years. Age, sex, mechanism, glasgow coma scale (GCS), systolic blood pressure (SBP), respiratory rate (RR), revised trauma score (RTS), injury severity score (ISS), pH, base excess (BE), as well as therapeutic interventions (i.e., angioembolization and number of blood units transfused in the first 24 h), were included in univariate and multivariate analyses by logistic regression of mortality predictive value.
Results
Overall mortality through the whole period was 17.2 %, and major respiratory morbidity in the ICU was 23.3 %. A significant increase of trauma admissions has been observed (before and after 2001, p < 0.01). Mean GCS (10.2) increased during the period (test trend p < 0.05). Mean age, ISS (24.83) and mechanism did not change significantly, whereas mortality rate decreased showing two marked drops, from 25.8 % in 1996, to 18.3 % in 2000 and again down to 10.3 % in 2004 (test trend p < 0.01). Traumatic brain injury (TBI) accounted for 58.4 % of the causes of death; hemorrhagic shock was the death cause in 28.4 % and multiple organ failure (MOF)/sepsis in 13.2 % of the patients. However, the distribution of causes of death changed during the period showing a reduction of TBI-related and increase of MOF/sepsis (CTR test trend p < 0.05). Significant predictors of mortality in the whole group were year of admission (p < 0.05), age, hemorrhagic shock and SBP at admission, ISS and GCS, pH and BE (all p < 0.01). In the subgroup of patients that underwent emergency surgery, the same factors confirmed their prognostic value and remained significant as well as the adjunctive parameter of total amount of blood units transfused (p < 0.05). Surgical time (mean 71 min) showed a significant trend towards reduction but did not show significant association with mortality (p = 0.06).
Conclusion
Mortality of severe trauma decreased significantly during the last 15 years as well as mean GCS improved whereas mean ISS remained stable. The new safety regulations positively influenced incidence and severity of TBI and seemed to improve the outcomes. ISS seems to be a better predictor of outcome than RTS.
Similar content being viewed by others
Background and aims
Every year, 1.2 million people are known to die in road traffic accidents (RTAs) worldwide. Millions more people sustain injuries leading to permanent disabilities. All countries worldwide are strongly affected in terms of mortality and morbidity, as well as of early or late consequences of traumatic injuries. Therefore, RTAs represent a major public health issue and the whole aims to develop preventive measures in order to decrease their incidence [1]. Road traffic injuries were the first cause of death in the 15–29 aged population in 2004 and still represent a major burden [2–6]. In Italy a consistent number of safety interventions have been adopted by the government in the last decades and have contributed to significant decrease incidence and severity of road crashes. These safety regulations started about a decade ago with compulsory use of helmets for motorbike drivers (2000) [7] and mandatory use of seatbelts for car drivers (2003) [8] as well as a penalty system for down-scoring driving license points until license withdrawal (2003) [9]. Further improvements have been attempted with more effective and strict enforcement on speed control (2007) [10] and alcohol consumption (2009) [11].
In light of the safety regulations adopted on a national scale in the last decade, we have assessed trauma epidemiology, outcomes and changes of care in our tertiary regional referral trauma center. Our experience in trauma management increased over time and improved with development of better logistics and optimization of structural and technical resources. In addition the above cited Government policy safety measures towards RTA prevention, decreased mortality rate for trauma and positively affected injury severity and outcomes.
The evaluation of the effects of these preventive measures and of the therapeutic strategies on mortality and causes of death during a 15-year period, and a careful analysis of predictive factors of mortality and morbidity, may lead to further improvements.
With this rationale and for this purpose, a Trauma Registry Database was established in our Trauma ICU (TICU) to record and subsequently analyze the severe trauma cases, and possibly, thanks to a Surgical Clinical Audit and peer review activity [12], improve the outcomes after adoption of focused interventions and measures.
Thus, the aim of the present study is to evaluate epidemiology of trauma in our regional referral Trauma Center during a 15-year period (1996–2010) and analyze the main indicators (age, sex, mechanism, glasgow coma scale (GCS), systolic blood pressure (SBP), respiratory rate (RR), injury severity score (ISS), revised trauma score (RTS), pH, base excess (BE), therapeutic interventions) and outcomes (mortality in ICU, causes of death, morbidity in ICU, LOS in ICU). We have also performed a trend analysis of the main indicators and outcomes through the years and therefore evaluated the timeline changes in light of recent safety measures. Finally, further aims are identification of prognostic factors significant predictors of mortality and outcome, for subsequent adoption of changes tailored on those factors susceptible of intervention, in order to improve clinical efficiency and care quality.
Material and methods
The region of Emilia Romagna covers an area of 22,446 km2 with 4,417,113 people. Bologna city and its suburbs have 984,342 inhabitants for a population density of 264/km2.
The positive effect of regionalization of trauma care has already been proven to significantly reduce delays, inadequate care, and preventable deaths [13].
Maggiore Hospital is a level I trauma center in Italy, being one of the three integrated trauma care systems (SIAT) in Emilia Romagna [14] and the highest level of regional tertiary referral centers for severe trauma (Fig. 1). The SIAT Trauma System was introduced in 2002 and authorized by the regional government with the aim of improving trauma care standards and outcomes [15]. Each SIAT works according to the Hub and Spoke model: highly specialized care services are available in the trauma center (Hub), which is connected to a network of rural hospitals (Spoke). Trauma patients are sent from Spoke to Hub to receive better quality of care. The main goal of SIAT is organization and management of efficient trauma care pathways and providing the most appropriate and fast treatment in major trauma patients. The main characteristics include delivery of full-range care to all injured patients in a defined geographic area, coordination with pre-hospital services, efficient use of resources through regionalization, population-based planning, and integration with the public health system for injury prevention [16]. Maggiore Hospital, with large volume of trauma cases and long-lasting experience, is an important national benchmark for trauma centers.
The pre-hospital care was given according to the standards of PHTLS and ATLS as well as to the European Trauma Course standards since 2010.
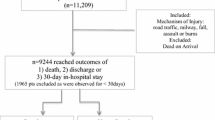
A total of 60,247 trauma admissions have been recorded in Maggiore Hospital between 1996 and 2010, with 2,183 deaths (Overall mortality 3.6 %). A total of 2,935 patients with severe polytrauma and ISS >16 have been admitted to TICUs and recorded in a prospectively collected database (1996–2010).
All severe trauma cases, defined as having an ISS of >16 and having therefore the criteria for being admitted to the TICU, have been included in this retrospective cross-sectional study. The data source was the Trauma Registry data bank of Maggiore Hospital Trauma Center. All available parameters were included in the analysis.
A retrospective review of outcomes has been carried out, including descriptive analyses, mortality rate, causes of death, morbidity and length of stay (LOS) in ICU, with stratification and analysis of outcome changes through the years. Trend analysis of the changes of all analysed factors has also been carried out. All available data and factors (i.e., age, sex, mechanism, GCS, SBP, RR, RTS, ISS, pH, BE, and therapeutic interventions as embolization and amount of blood units transfused in the first 24 h), were included in univariate and multivariate analyses (Cox logistic regression) of mortality predictive value.
The statistical analysis was conducted using statistical software package (SPSS 13.0®). Data are expressed as numbers (%) and means (standard deviation [SD]). The results were analyzed using chi-square test and Fisher exact test, as appropriate, for proportions in case of discrete data. For means, in case of continuous numerical data, independent-samples t-test and Mann–Whitney test have been used respectively for normally and non-normally distributed data (data were previously tested for normality by Kolmogorov–Smirnov test). Chi-square test (significance for 95 % confidence interval [CI]) was used for testing the association between the analyzed characteristics, whereas influence of each factor on mortality has been evaluated by odds ratio (OR) using Mantel–Heantzel test. The significant factors after univariate analysis have been therefore tested by multivariate (logistic regression) analysis [17].
Kaplan–Meier curves were used for overall survival analysis and its significance has been tested using Log-rank (Mantel–Cox) test. The differences were in any case considered statistically significant with p value of <0.05.
The statistical significance of temporal changes (timeline 1996–2010) of patient's characteristics and outcomes has been tested using Cochran–Armitage trend test.
Results
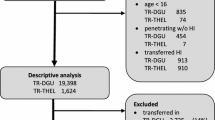
The sex distribution of severe trauma population showed strong prevalence of males (74.8 % vs. 25.2 % females). Mean age of the 2,935 trauma patients with ISS >16 and admitted to the TICU was 44.12 years (median 39, SD 21.1). Whilst in the overall trauma patients population admitted to the emergency department (ED) of our trauma canter, incidence of penetrating trauma is 9.8 % (1996–2010) vs. 90.2 % blunt cases, within those 2,935 patients with ISS >16 and admitted to the TICU, the injury mechanism showed overwhelming prevalence of blunt trauma (97.1 %), whereas only 2.5 % penetrating and 0,4 % other mechanisms. The most common setting of injury was RTA (72 %), followed by accidents in the workplace (7 %) and suicide attempts (5 %) (Fig. 2). Trough the whole study period, overall trauma admissions significantly increased and incidence of trauma admissions in TICU significantly raised after 2001 (before vs. after 2001, test trend p < 0.01) (Fig. 3). However, although fluctuating, the incidence of RTA did not significantly change during the years of the study (test trend p = ns) (Fig. 4). On the other hand a significant increase of penetrating trauma and workplace accidents has been recorded. A total of 523 patients (17.8 %) presented hypovolemic shock at admission whereas 82.2 % of the patients were hemodynamically stable. Two hundred twenty patients (7.5 %) were also hypothermic at admission (defined as body temperature <35 °C). Physiologic status of the patients is reported in Table 1; during the first 24 h in the ICU, the average amount of 2.6 blood units was transfused (median 1.5, SD 33,3), whilst the average total number of blood units transfused during whole ICU stay was 4,1 per patient (median 2.5, SD 15.6) (Table 1). Mean GCS was 10.2 (median 12, SD 4.9), and its distribution showed three main peaks of incidence, respectively scores of 14–15, 6-7-8 and GCS 3 (Fig. 5). Mean GCS significantly increased and improved during the period (test trend p < 0.05) (Fig. 6). Mean age, ISS (mean 24.83) and mechanisms of injury did not have significant temporal change (Table 1 and Fig. 7).
Overall ICU mortality in the whole period was 17.2 %, major respiratory morbidity in the ICU 23.3 %. The mean LOS in the ICU was 11.1 days (median 5, SD 51.3).
Notably, mortality rate significantly decreased showing two marked drops, from 25.8 % in 1996, to 18.3 % in 2000 and again down to 10.3 % in 2004 (test trend p < 0.01) (Fig. 8). Mortality for trauma in TICU population reached the lowest rate of 9.4 % in 2008, rising again to 13.3 % in 2009 (Fig. 8). Traumatic brain injury (TBI) accounted for 58.4 % of causes of death, hemorrhagic shock in 28.4 % and MOF/sepsis in 13.2 %. However, the distribution of causes of death changed during the period showing reduction of TBI-related mortality, although TBI did remain first cause of death; meanwhile, an increase of deadly MOF/Sepsis has been recorded (CTR Test Trend p < 0.05) (Fig. 9). Hemorrhagic shock has remained fairly constant as mortality cause through the study period, with a small, not significant decrease in recent years (Fig. 9).
Significant predictors of ICU mortality in the whole group were year of admission (p < 0.05), age, hemorrhagic shock and initial SBP (p < 0.05), GCS (p < 0.02), ISS, RTS and tissue perfusion indicators (i.e., pH and BE) (all factors p < 0.01). After multivariate analysis, hemodynamic status-related parameters (hemorrhagic shock and SBP, pH and BE), GCS, ISS and age remained the strongest significant predictors of mortality (Table 2).
A total of 1,601 patients (54.5 %) needed emergency surgery. In the subgroup of patient that underwent emergency surgery, the same factors confirmed to be significantly associated with mortality in addition to the number of blood units transfused (p < 0.05) (Table 3). Average duration of surgery was 71 min (median 59, SD 198), showing a significant trend towards reduction in recent years (p < 0.05). Duration of surgery showed nearly significant influence (p = 0.06) on mortality, although not statistically significant. Significant reduction of surgical times has been observed for all specialties, including neurosurgical, orthopaedics and thoraco-abdominal surgeries. The most significant decrease has been recorded in trunk and abdominal trauma procedures, with a larger use of Damage Control Surgery. After multivariate analysis, prognostic factors predictive of overall mortality in subgroup of surgically treated patients were age, hemorrhagic shock, SBP, pH, BE, GCS, ISS and amount of blood units transfused (Table 3).
Discussion
The European Union policy aimed to reduce deaths for RTA by up to 50 % within 2001–2010 [18, 19]. Within the policy of road injuries prevention, an act was issued by the European Commission in 1997 (Act 131): "Promoting road safety in the EU: the program for 1997–2001" [20]. In Italy, this act was adopted 2 years later (National Road Safety Plan [PNSS] 1999; Act 144) [21].
Several safety measures (such as helmet, seatbelts, airbags, child restrains) have been therefore adopted for reducing incidence of death or serious injuries after RTA. In the last decade, three cornerstone measures have been adopted by Italian government for safety improvement. In year 2000, helmets were declared compulsory, and use of lighter open-face helmets (so-called Cromwell) has been prohibited. In 2003, seatbelts were also declared mandatory and further safety regulations, including child restrains, have been adopted for children. In the same year, a penalty system for speed limits, down-scoring overall points and leading to driving-license withdrawal, has also been introduced.
In Italy, safety measures have been underused. From December 2000 to June 2002, among 2253 K observations, only 32.1 % of drivers fastened their seatbelts (40.8 % in northern compared to 20.2 % in southern Italy) [22].
The beneficial effect of the safety regulations issued in 1999 led to wider helmet use: 81.2 % in northern and 70 % in southern Italy.
A study from Veneto Region showed a decreased trend of indicators "number of injuries" and "mortality" before and after the law for down-scoring driving license credits. The introduction of penalty points was associated with decreased trend of injuries (p < 0.001), (almost constant in previous periods), and with substantial decrease of deaths. After adoption of the new regulations, overall reduction in 18-month prediction (July 2003–December 2004) was around 9 %, with 37,469 injured people observed and 41,051 expected [23].
Assessment of helmet use and TBI, before and after the introduction of new rules in Romagna region, found that helmet use increased from less than 20 % in 1999 to over 96 % in 2001 and it was an effective measure for preventing TBI in all age groups [24].
National data from the Trauma Data-Bank of Italian National Institute for Statistics (ISTAT) [25] published in 2008 [26] confirmed a constant reduction of mortality rates in the last 30 years, which is even more meaningful given the increased incidence in Italy of overall trauma events RTA-related of any severity; incidence of RTA increased more significantly in the last 15 years.
ACI-ISTAT has recently provided new data [27]. In 2009, traffic accidents in Italy were 215,405, resulting in 4,237 deaths and 307,258 injuries of different severity. Compared to 2008, there is a decreased number of accidents (−1.6 %) and injuries (−1.1 %) and a more substantial decrease of deaths (−10.3 %). Between 2001 and 2009, traffic accidents with major personal injuries decreased from 263,100 to 215,405 (−18.1 %), deaths decreased from 7.096 to 4.237 (−40.3 %) and injuries from 373,286 to 307,258 (−17.7 %). It should be emphasized that during the same period, road traffic has grown by about 18 %. Therefore, a lower proportion of severe trauma among overall incidence of RTA, may be hypothesized.
In our population, although Trauma admissions increased, RTA and ISS remained constant; overall mortality and TBI decreased significantly.
Occurrence of RTAs and mortality improved overall, as a direct consequence of government's efforts towards safety. Perhaps, a significant development in clinical management skills in the Italian trauma centers, more effective logistics and organization in the Trauma referral network (such as SIAT system), may be acknowledged.
For this purpose, the Haddon matrix shows how to prevent and how to improve all the critical variables of the system. By utilizing this framework, the relative importance of different factors may be evaluated and interventions may be designed [28].
After comparing the findings from our large trauma population with nationwide data from ISTAT, we have therefore compared our results with other population-based surveys.
An interesting study focusing on similar issues is reported by the Adams Cowley Shock Center, University of Maryland Medical System. The analysis of trauma mortality pattern (1997–2008), showed that overall survival has not improved, in spite of advances in trauma care. Although overall survival has not improved, it remained stable in a population being both older and more severely injured [29].
Specifically, we have reviewed comparatively the Maryland experience (68,454 admissions for trauma in the period 1996–2008) with our database (1996–2010). The annual number of admissions increased by roughly 2 %/year (p < 0.001). A drop in admissions in FY 2008 (5,060 vs. 6,263 in 2007) decreased the overall slope of this increase to roughly 1 % (p = 0.15). Mortality through this era ranged from 3 % to 3.7 % and overall slightly worsened (p = 0.04). However, among those patients admitted with ISS 17–25, survival improved significantly (p = 0.0003). Overall mortality in this study was 3.4 % (Trauma patients of any ISS) and, not surprisingly, mortality was associated with increasing age and ISS.
As a comparison, in our region through the study period both overall trauma admissions in Maggiore Trauma Center and TICU admissions significantly increased (the latest after 2001; Fig. 3). However, although fluctuating, the incidence of RTA has not significantly changed during the study period (Fig. 4), most probably following national trauma prevention policy. Overall mortality of all Trauma admissions in our Center (60,247 admissions between 1996 and 2010) has been 3.6 %, comparable to the above reported US experience. Among 2935 patients with ISS >16, overall mortality was 17.2 %.
In our series and regional setting, the regulations of government policy on road safety did not lead to decreased number of accidents and this data matches national data (Fig. 10). However, we have observed in our population a decreased mortality (from 25.8 % in 1996 to 13.3 % in 2009) with multi-steps falls: the first in 2000, second in 2004 and third in 2008. Accordingly, in the national setting, a continuous decrease in mortality has been recorded during the last decade (Fig. 11): mortality rate drop of 10.3 % in 2009 with respect to 2008 and 40.3 % from 2001 (source ISTAT).
These results are in keeping with the expected benefits of EU policy new regulations aimed to reduce deaths for RTA up to 50 % within 2001–2010.
Brain injury is historically the main cause of death for trauma worldwide. Wearing a motorcycle helmet reduces the risk of death by almost 40 % and the risk of severe injury by 70 % [30]. The "GLOBAL STATUS REPORT ON ROAD SAFETY", published by WHO in 2009, draws attention to this problem, highlighting that “Only 40 % (178 Country analyzed) have a motorcycle helmet laws, helmets should meet a specific national or international standard” [31].
In 2003, the Italian government widened regulatory restrictions on helmet use, prohibiting the so called "Cromwell" model; the effectiveness of motorcycle helmets in reducing head injuries is in part a result of the helmets quality. Requiring helmets to meet a safety standard may effectively reduce the impact of head collision in case of crash [32, 33].
In our TICU population, TBI accounted for 58.4 % of the causes of death, hemorrhagic shock in 28.4 % and MOF/sepsis in 13.2 %. We have also found similar values in the study from Dutton et al. [27], where TBI accounted for 51,6 % of deaths, acute hemorrhage for 30 %, MOF for 10,5 %, and other/indeterminate causes for 7,9 %. In this study, although overall mortality slightly worsened, decreased mortality was observed in the group of severely but not lethally injured patients (ISS of 17–25).
We have had a similar trend in our population. The distribution of death causes markedly changed in our population, showing a reduction of TBI-related, although still remaining first cause of death. This data, together with the improvement of average admission GCS (more remarkable after 2006), may be related to the beneficial effects of several regulations on helmet use adopted in previous years, although average overall severity (measured by ISS) has not decreased.
Dutton reported that the median time to death for uncontrollable hemorrhage, TBI, multiple organ failure was 2 h, 24 h, and 15 days, respectively. TBI deaths were mostly associated with blunt trauma (71.3 %), bleeding deaths with penetrating trauma (59.8 %), and MOF, overwhelmingly, with blunt trauma (89.3 %). Conversely, blunt trauma was mainly associated with death TBI-related (56.6 %). These patterns did not change significantly over time [27].
In our database, we have recorded increase of MOF/Sepsis as main cause of mortality. As regards sepsis, because of worldwide overuse and misuse of antibiotics, common bacteria are becoming resistant. This is a major concern since several studies showed that inappropriate antibiotics prescription is regrettably a common use and not the exception; as a result this would lead to significant morbid consequences in terms of costs and public health [34].
The incidence and the constant or even increasing rate of MOF can be easily explained because MOF and sepsis are most often direct consequences of polytrauma and hypovolemic shock itself, especially if the shock is prolonged.
Probably the constant incidence of hypovolemic shock, although changes in the severity of trauma and improvements in pre-hospital care occurred, may be explained with changing paradigms in the aggressive resuscitation policy. In the past decades, the tendency was towards a more aggressive fluids administration policy, aiming to raise and to maintain the SBP on or above 90 mmHg, even with liberal use of more than 10 L of colloids and/or crystalloids. In the last decade, the policy had a shift towards the concepts of permissive hypotension and goal-directed resuscitation, based on strict transfusion protocol, based on the following ratio: RBCs/FFP/platelets pack 2.5:2:1
Again, Dutton reported the proportion of males admitted remained stable (roughly 70 %). Blunt injury was overwhelmingly the most common throughout the whole study period (roughly 80 %, 60 % associated with motor vehicles). However, the proportion of injuries due to blunt impact also increased (p = 0.01), mainly because of significant increase in admissions for falls (p = 0.002). Overall admissions for penetrating injury remained statistically stable (p = ns) despite significant decrease in admissions for gunshot wounds and stabbings (p < 0.001 for both).Overall, men were significantly younger and more severely injured than women but age and injury severity increased significantly during the study period, both overall and gender-related. ISSs worsened significantly throughout the years for both blunt and penetrating trauma, mainly associated with significant changes in severity scores for MVA-related injuries and gunshot wounds.
In comparison, our results showed a strong prevalence of males (74.8 %). The injury mechanism showed strong prevalence of Blunt trauma (97.1 %), higher than observed in the overall trauma population (90.2 %). This is in keeping with epidemiology and mechanisms of trauma in Western European countries. The most common setting of injury was road traffic (Fig. 2).
The incidence of RTA has not significantly changed throughout the years of the study (Test-Trend p = ns) (Fig. 4). On the other hand a significant increase of penetrating trauma and workplace accidents has been recorded. A significant increase in the incidence of penetrating injuries has already been observed in the most recent years in our trauma center. In fact, penetrating trauma doubled in the period 1989–2008 from 4.17/year up to 8.53/year, accounting now for 13.95 % of all trauma laparotomies vs. 7.8 % in the previous decade. Interestingly, a strongly significant change has been observed in demographics of the victims (67.2 % were extra-EU origin vs. 8 % in previous decade, p < 0.01) [35].
In our population, average ISS remained fairly constant through the years, despite the decreased mean GCS (following wider use of helmet and seatbelts); this may be explained because average AIS severity of other districts (chest/abdomen/extremity) did not change in these severely injured patients, such those referred to our tertiary trauma center.
Interestingly, a statistically significant higher median ISS (32 vs. 24) has been observed in the subgroup of ICU patients with penetrating mechanism vs. ICU patients with blunt trauma. This may be due to the higher incidence of Gunshot Wounds among the penetrating trauma patients who needed ICU admittance (78 % of the penetrating TICU population were GSW related). Nevertheless in the overall trauma patients population, most of the penetrating cases were Stab Wounds (82 %), meaning that overall incidence of penetrating trauma in TICU patients is lower than in the general trauma patients dataset but has an higher incidence of GSW mechanism (higher severity).
In our multivariate analysis of prognostic factors, hemodynamic status, SBP and indicators of tissue perfusion (pH and BE) reached high significance, suggesting that appropriate resuscitation and effective transfusion protocol may be primary targets for improving treatment.
The rFVIIa trauma trial [36] identified an association between RBC transfusion and development of multiple organ failure (MOF), which was already known [37]. In particular, transfusion >10 RBC units from arrival to 24 h is associated with increased mortality; this threshold was also identified previously [38]. Nevertheless, there is statistically variation between countries with respect to adherence to the RBC transfusion guideline as well as resuscitation fluid therapy (colloids vs. crystalloids). A defined and common protocol has never been used, but differences in clinical outcomes may also result from differences in patient management34. Knowledge of such variation is critical for enhancing patient care because of their potential influence on clinical outcomes. Here is why it is crucial to identify specific areas, target for education and intervention.
In a survey from the National Trauma Data Bank (2002–2006) including patients with at least one severe injury (Abbreviated Injury Scale score, ≥3) from level I and II trauma centers (217,610 patients, 151 centers), significant variations in risk-adjusted mortality rates were noted across centers [39]. Large variations in LOS were also noted, with the median ranging from 4 to 8 days. Independent predictors of prolonged LOS included gunshot-wound mechanism, ISS, admission to ICU, preinjury comorbidities, and occurrence of complications. Among complications, infections, pulmonary embolism, cardiovascular and respiratory complications were the most important determinants of LOS.
Mean length of ICU stay was 11.4 days in our study, with overall mortality of 17.3 %; mortality was due to MOF/sepsis in 13.2 % of cases with a significant trend towards increased incidence of deadly MOF/sepsis. Incidence of major respiratory and ventilation-related morbidity in ICU has been 23.3 %.
In the CONTROL trial [34], prospective double-blinded multicenter RCT (100 hospitals, 20 countries) comparing rFVIIa with placebo in severe trauma patients with refractory bleeding, significant predictors of 24-h mortality were RBC >10 units between admission and 24 h, admission lactate >5 mmol/l, chest AIS score > 4 and overall non-adherence to clinical guidelines. Significant predictors of 24 h to 90 days mortality were age >60 years, male gender, admission lactate >5 mmol/l, admission hemoglobin <10 g/dl, highest AIS score = 5 and overall non-adherence to guidelines. Significant predictors of 90 days mortality were age >60 years, male gender, RBC >10units, admission lactate >5 mmol/l, admission hemoglobin <10 g/dl and overall nonadherence to guidelines.
Similarly, in our study, significant predictors of mortality were year of admission (p < 0.05), age, hemorrhagic shock, SBP, ISS, RTS, GCS and tissue perfusion indicators (all factors p < 0.01). However in the subgroup of patient underwent surgery, the number of blood units transfused was significant predictor of mortality also in our population.
On average, among the CONTROL Trial participating centers, damage-control-surgery guideline was less well adhered to, than the RBC transfusion and ventilator guidelines. Also significant variation occurred among countries in adherences to RBC transfusion guidelines.
Since the indicators of tissue perfusion (pH, BE) resulted strongly predictive of outcome in our series, an aggressive fluid resuscitation and appropriate transfusion protocol (the RBC/FFP/platelets ratio used in Maggiore Hospital is 2.5:2:1) together with early surgical consultation and appropriate treatment with damage control surgery when necessary, are therefore advisable for improving outcomes.
A critical review from Los Angeles County University of Southern California Medical Center, of 2,081 deaths during initial hospital admission (1998–2005) among 35,311 trauma patients (5.9 %), demonstrated that delay in treatment and error in judgement are leading causes of preventable and potentially preventable deaths [40]. In this series, for the 51 patients whose deaths were classified as preventable/potentially preventable, mean age was 40 years, 66.7 % were men, mechanism of injury was blunt in 74.5 %, mean ISS was 27, mean admission SBP was 110 mmHg, and mean admission GCS was 12. Overall, 13.7 % of the patients had hypotension (SBP <90 mmHg) and 23.5 % had a GCS score of 8 at admission. The most common death cause was bleeding (39.2 %) followed by MOF (27.5 %), and cardiorespiratory arrest (15.6 %). Interestingly, preventable or potentially preventable deaths peaked at two time periods: 51.1 % during the first 24 h and 31.4 % after 7 days; deaths most commonly occurred in the ICU (54.9 %). These data and patient characteristics, mostly comparable to our results, suggest that a relevant percentage of patients with good parameters at admission, such as SBP and GCS, may be affected by high incidence of early and late mortality, mainly related to hemorrhage and MOF/sepsis, respectively, suggesting an aggressive resuscitation and prevention of MOF/sepsis to be the main targets for decreasing morbidity and mortality.
Duration of the surgical procedures showed a significant trend towards reduction in the recent years and a probable, although not statistical significant in our database, positive effect on survival. As already highlighted, reduction of surgical times has been observed for all types of surgery but mostly in trunk and abdominal trauma procedures, in keeping with damage-control-surgery philosophy. DCS became an inevitable strategy in treating severely traumatized patients [41]. The rationale for DCS is that mortality in surgical patients who develop hypothermia, acidosis and coagulopathy (lethal triad) is extremely high unless patients' physiologic stability is re-established [42, 43].
DCS involves three distinct stages. In the first stage, rapid temporary measures are taken to control bleeding and contamination, followed by rapid abdominal closure. The second involves aggressive correction of lethal triad in ICU. The third is planned re-operation for definitive repair of injuries [44–46]. Indeed, is now well recognized that multiple trauma patients are more prone to die from their intra-operative metabolic failure than from failure of complete operative repairs [47, 48]. Patients with major exsanguinating injuries will not survive complex procedures such as a formal hepatic resection or pancreaticoduodenectomy. The operating team must undergo a paradigm shift in their "mindset" if the patient is to survive such devastating injuries [49].
The appropriate use of this strategy can lead to a reduction of morbidity and mortality in unstable complex trauma patients, either blunt or penetrating [50]. On the other hand, a routine laparotomy is not indicated in hemodynamically stable patients without signs of peritonitis or diffuse abdominal tenderness. Mandatory laparotomy for penetrating abdominal trauma detects some unexpected injuries earlier and more accurately, but results in higher non-therapeutic laparotomy rate, leading to complications, longer LOS and increased cost. Thus, while non-operative management (NOM) of blunt trauma is now the gold standard, management of penetrating trauma is still controversial. Recently, increased use of NOM and laparoscopy contributed in decreasing incidence of unnecessary laparotomies as well as overall morbidity and mortality [33].
Subsequently, this may be interpreted in our findings, showing a significant reduction of surgical times (from 91 to 49 min) observed for all types of surgery, including neurosurgical, orthopaedics and thoraco-abdominal surgeries. Perhaps, although duration of surgery did not reach a statistically significant association with mortality, it probably does play a relevant role since it was nearly significant (p = 0.06).
Last but not least, as in other countries, the positive effect of regionalization and trauma-center care system has contributed to improve the outcomes, since the integrated SIAT system has started in Emilia Romagna in 2002.
Better outcomes are achievable in level I trauma centers as shown in Ohio State Trauma Registry: overall mortality was 7.7 % in level I Trauma Centers (36 % ISS >15) vs. 7.2 % in level II (22.2 %, ISS >15, OR = 0.75). Better survival was confirmed in the seriously injured (ISS >15) group (19 % vs. 24.1 %, OR = 0.76) [51]. Similar results were reported in Oregon, where trauma patients transferred from nontertiary EDs to major trauma centers had lower in-hospital mortality than patients remaining in nontrauma hospitals; mortality was 8 % in Level I TC (mean ISS 15.2) vs. 4 % in rural hospitals (mean ISS 10) [52].
Similarly, a national US evaluation of trauma center care effect on mortality, including 18 level I trauma centers and 51 rural hospitals with 5,191 patients, whose roughly 50 % sustained blunt MVA trauma and 53 % had ISS >15, found in-hospital mortality to be significantly lower at TC (7.6 % vs. 9.5 %) as well as 1-year mortality (10.4 % vs. 13.8 %) [53]. Conversely the EuroTARN group showed significantly worse outcome within European Trauma Registries [54]; among 96,084 cases from 14 countries, 96 % had blunt injury, 55 % from RTA, and 21.582 (22 %) had ISS > 15 and the overall mortality ranged from 13 % to 56 %.
Worse results in European settings, where organized trauma system is often lacking, were confirmed in 35,564 blunt trauma cases in the UK; 33 % sustained RTA and 23 % had ISS > 16. As expected, median age was 46 years and 63 % were men. 7 % of patients died before discharge but in the group with ISS >16 mortality reached 23 % [55].
A recent report confirmed that management of severely injured patient with associated head injury in England and Wales (data from TARN), where an organized trauma system is absent, was associated with increased crude and risk-adjusted mortality (OR = 2.15 and 3.22, respectively) compared with inclusive trauma system in Victoria, Australia [56]. This comparative review included 4,064 and 6,024 trauma patients with ISS >15, respectively from Australia and UK, having sustained RTA in 54 % of the cases, with mean SBP at admission around 140 mmHg, and roughly GCS score of 13–15 in 50 %.
However, improved outcomes have been reported in Europe after regionalization of trauma care with institution of specialist multidisciplinary trauma service and performance improvement program; in fact mortality from critical injury at Royal London Hospital was 48 % lower in 2005 than 2000 (17.9 % vs. 34.2 %; p = 0.001) [57].
A comparative table showing differences of characteristics and outcomes of several Trauma populations from different US and European Trauma Registries is shown in Table 4.
Conclusions
Although uncontrolled variables such as different referral patterns, changing population characteristics, retrieval methods and protocols, admission thresholds for intensive care, and definition/coding errors may affect the interpretation of the present study, this is one of the largest population cross-sectional survey studies reporting trauma epidemiology and outcomes.
In our large population-based study, increased incidence of trauma admissions (ISS >16) in the TICU has been observed in the last 15 years. Mortality of severe trauma significantly decreased, mean GCS improved whereas ISS remained stable. A significant change in causes of death has been also recorded, TBI decreased and MOF/sepsis increased. Age, hemodynamic status, ISS, pH, BE, GCS are the strongest prognostic predictors of mortality. ISS, traditionally recognized as the first predictive trauma score [58], seems in our study to be better performing predictor of outcome than RTS. The newly issued safety regulations, positively influenced incidence and severity of TBI and seemed to improve the outcomes. These patterns may suggest that efforts towards carefully planned and widely adopted social preventive measures, may improve outcomes and lead to tailored deployment of new treatments or improvement of existing ones. Such policy is therefore advisable and these issues need to be addressed. Indeed, most trauma deaths occurs in the immediate post-injury period. These patients usually die on the scene or during transport from overwhelming injury such as spinal cord transaction, aortic disruption or massive intra-abdominal injuries. Despite modern emergency medical systems networks, there is little that sophisticated treatment systems can do to save these patients, thus, efforts should be directed at prevention. Dramatically improving therapy in a modern trauma system may decrease trauma mortality by 13 % [59]. In contrast, more than half of all deaths are potentially preventable with preinjury behavioral changes. Injury prevention is critical for reducing deaths in modern trauma systems. Deaths usually caused by severe TBI or uncontrolled hemorrhage, occur within hours and represent preventable deaths. Teixera demonstrated that protocols implementation to decrease human error (especially delay in treatment and error in judgment) and system changes such as regionalization of care are able to improve quality of trauma care as measured by a decrease in preventable trauma deaths [38]. Differently from USA, Italy lacks a "Trauma Quality Improvement Program" and especially of a consolidated fellowship in surgical and acute critical care. For this reason, the resources should be joined and efforts made to create a common "vision" for the future of emergency care, including the development of specialized institution with dedicated physicians, in order to achieve a common culture of trauma with defined standards on critical care and achieve appropriate preventive and therapeutic strategies, as recently highlighted in the Report from Critical Care Committee of American Association for Surgery of Trauma [60]. Guidelines for critical care medicine training and continuing medical education ease standards on critical care. These standards are the basis for establishing a comparison and understand if we really are doing better.
References
Peden M (2004) World report on road traffic injury prevention—summary. World Health Organization, Geneva, p 12
Racioppi F et al (2004) Preventing road traffic injury: a public health perspective for Europe. Copenhagen, WHO Regional Office for Europe
The global burden of disease: 2004 update. Geneva, World Health Organization, 2008 (http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_AnnexA.pdf)
http://www.euro.who.int/__data/assets/pdf_file/0015/43314/E92789.pdf
http://www.who.int/violence_injury_prevention/road_safety_status/2009/en/
Di Saverio S, Sibilio A, Biscardi A. et al. A proposed algorithm for multimodal liver trauma management from a surgical trauma audit in a Western European trauma center, Minerva Aneshesiologica, In press
Hackford SR, Hollingworth-Fridlund P, Cooper GF, Eastman AB (1986) The effect of regionalization upon the quality of trauma care as assessed by concurrent audit before and after institution of a trauma system: a preliminary report. J Trauma 26:812–820
http://asr.regione.emilia-romagna.it/trauma/en/siat/index.htm accessed on Sep 13th 2013
http://asr.regione.emilia-romagna.it/trauma/en/trauma_registry/index.htm accessed on Sep 13th 2013
J Hammond (2008) Trauma systems, triage and disaster management. Surgery Section Two, 403–408. DOI:10.1007/978-0-387-68113-9_21
Hosmer DW (2000) Lemeshow S Applied logistic regression. Wiley
http://ec.europa.eu/transport/road_safety/specialist/policy/index_en.htm
http://www.euro.who.int/__data/assets/pdf_file/0008/98423/E91710.pdf
http://europa.eu/legislation_summaries/transport/road_transport/l24055b_en.htm
http://www.iss.it/binary/sicu/cont/LIBRO%20II%20(296–299)%20SITO.1115814066.pdf
Servadei F et al (2003) Effects of Italy’s motorcycle helmet law on traumatic brain injuries. Inj Prev 9:257–260
http://www.istat.it/dati/catalogo/20081112_00/contenuti.html
http://www.istat.it/salastampa/comunicati/non_calendario/20081120_00/testointegrale20081120.pdf
Haddon W Jr (1999) The changing approach to the epidemiology, prevention, and amelioration of trauma: the transition to approaches etiologically rather than descriptively based. 1968. Inj Prev 5(3):231–5
Dutton RP, Stansbury LG, Leone S, Kramer E, Hess JR, Scalea TM (2010) Trauma mortality in mature trauma systems: are we doing better? An analysis of trauma mortality patterns, 1997–2008. J Trauma 69(3):620–6
Liu B et al (2005) Helmets for preventing injury. Cochrane Database Syst Rev( issue 4)
http://whqlibdoc.who.int/publications/2009/9789241563840_eng.pdf
http://www.who.int/violence_injury_prevention/publications/road_traffic/helmet_manual.pdf
Spiritus E (2000) Antibiotic usage for respiratory tract infections in an era of rising resistance and increased cost pressure. Am J Manag Care 6(Suppl 23):S1216–S1221
Casali M, Di Saverio S et al (2008) Penetrating abdominal trauma: 20 years experience in a Western European Trauma Center. Ann Ital Chir 79:399–407
Christensen MC, Parr M, Tortella BJ, Malmgren J, Morris S, Rice T, Holcomb JB, CONTROL Study Group (2010) Global differences in causes, management, and survival after severe trauma: the recombinant activated factor VII phase 3 trauma trial. J Trauma 69(2):344–52
Moore FA, Moore EE (1997) Blood transfusion: an independent risk factor for post-injury multiple organ failure. Arch Surg 132:620–625
Tien H, Nascimento B Jr, Callum J, Rizoli S (2007) An approach to transfusion and hemorrhage in trauma: current perspectives on restrictive transfusion strategies. Can J Surg 50(3):202–9
Shafi S, Barnes S, Nicewander D, Ballard D, Nathens AB, Ingraham AM, Hemmila M, Goble S, Neal M, Pasquale M, Fildes JJ, Gentilello LM (2010) Health care reform at trauma centers—mortality, complications, and length of stay. J Trauma 69(6):1367–71
Teixera PGR, Inaba K, Demetriades D et al (2007) Preventable or potentially preventable mortality at a mature trauma center. J Trauma 63(6):1338–346
Baldoni F, Di Saverio S et al (2011) Refinement in the technique of perihepatic packing: a safe and effective surgical hemostasis and multidisciplinary approach can improve the outcome in severe liver trauma. Am J Surg 201(1):e5–e14
Ikegami K, Yamada K, Morimoto F, Kamohara T (2002) Sato Y Pathophysiologic changes in trauma patients and indications of damage control surgery. Nippon Geka Gakkai Zasshi 103(7):507–10
Filicori F, Di Saverio S et al (2010) Packing for damage control of nontraumatic intra-abdominal massive hemorrhages. World J Surg 34(9):2064–8
Poortman P, Meeuwis JD, Leenen LP (2000) Multitrauma patients: principles of 'damage control surgery. Ned Tijdschr Geneeskd 144(28):1337–41
Rotondo MF et al (1997) The damage control sequence and underlying logic. Surg Clin N Am 77:761–78
Moore EE (1996) Staged laparotomy for the hypothermia, acidosis and coagulopathy syndrome. Am J Surg 172:405–410
Rotondo MF, Schwab CW, McGonigal MD et al (1993) Damage control — an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 35:375–382
Hirshberg A, Mattox KL (1995) Planned reoperation for severe trauma. Ann Surg 222:3–8
Damage Control Surgery, Karim Brohi, trauma.org 5:6, June 2000
Tugnoli G, Casali M et al (2007) The damage control surgery. Ann Ital Chir 78(2):81–84
Cudnik MT, Newgard CD, Sayre MR, Steinberg SM (2009) Level I versus Level II trauma centers: an outcomes-based assessment. J Trauma 66(5):1321–6
Newgard CD, McConnell KJ, Hedges JR, Mullins RJ (2007) The benefit of higher level of care transfer of injured patients from nontertiary hospital emergency departments. J Trauma 63(5):965–71
MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO (2006) A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 354(4):366–78
Edwards A, Di Bartolomeo S, Chieregato A, Coats T, Della Corte F, Giannoudis P, Gomes E, Groenborg H, Lefering R, Leppaniemi A, Lossius HM, Ortenwal P, Roise O, Rusnak M, Sturms L, Smith M, Bondegaard Thomsen A, Willett K, Woodford M, Yates D, Lecky F (2007) A comparison of European Trauma Registries. The first report from the EuroTARN Group. Resuscitation 75(2):286–97
Christensen MC, Ridley S, Lecky FE, Munro V, Morris S (2008) Outcomes and costs of blunt trauma in England and Wales. Crit Care 12(1):R23
Gabbe BJ, Biostat GD, Lecky FE, Bouamra O, Woodford M, Jenks T, Coats TJ, Cameron PA (2011) The effect of an organized trauma system on mortality in major trauma involving serious head injury: a comparison of the United Kingdom and Victoria, Australia. Ann Surg 253(1):138–43
Davenport RA, Tai N, West A, Bouamra O, Aylwin C, Woodford M, McGinley A, Lecky F, Walsh MS, Brohi K (2010) A major trauma centre is a specialty hospital not a hospital of specialties. Br J Surg 97(1):109–17
Baker SP, O'Neill B (1976) The injury severity score: an update. J Trauma 16:882–885
Stewart RM, Myers JG, Dent DL, Ermis P, Gray GA, Villarreal R, Blow O, Woods B, McFarland M, Garavaglia J, Root HD, Pruitt BA Jr (2003) Seven hundred fifty-three consecutive deaths in a level I trauma center: the argument for injury prevention. J Trauma 54(1):66–70, discussion 70–1
Napolitano LM, Fulda GJ, Davis KA, Ashley DW, Friese R, Van Way CW, Meredith JW, Fabian TC, Jurkovich GJ, Peitzman AB (2010) Challenging issues in surgical critical care, trauma, and acute care surgery: a report from the Critical Care Committee of the American Association for the Surgery of Trauma. J Trauma 69(6):1619–33
Acknowledgments
Authors' own personal work; the data are extracted from the Clinical database of our TICU in Maggiore Hospital Trauma Center (http://asr.regione.emilia-romagna.it/trauma/en/siat/index.htm and http://www.riaonweb.it/Documenti/trauma_web/traumaweb.html).
Author contributions
Conception and design: S. Di Saverio, G. Gambale, G. Tugnoli, G. Gordini
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: Salomone Di Saverio, Federico Coccolini, Fausto, Eleonora Giorgini, Luca Ansaloni, Niki Amadori, Stefano Magnone, Filippo Filicori, Carlo Coniglio, Aimone Giugni, Andrea Biscardi, Piergiorgio Cavallo, Silvia Villani, Francesco Cinquantini, Giovanni Gordini, Gregorio Tugnoli
Provision of study materials or patients: G. Gordini, G. Tugnoli, G. Gambale, M. Annicchiarico, C. Coniglio
Collection and assembly of data: S. Di Saverio, G. Tugnoli, E. Giorgini, C. Coniglio, A. Giugni, P. Cavallo, G. Gambale, G. Gordini.
Data analysis and interpretation: S. Di Saverio, E. Giorgini, F. Catena, G. Tugnoli.
Manuscript writing and discussion: S. Di Saverio, G. Gambale, G. Tugnoli, E. Giorgini, N. Amadori
Correction and drafting: S. Di Saverio, E. Giorgini, N. Amadori
Revision for important intellectual content: S. Di Saverio, G. Gambale, F. Coccolini, F. Catena, G. Tugnoli, G. Gordini
Final approval of manuscript: Salomone Di Saverio, G. Gambale, F, Coccolini, Fausto Catena, Eleonora Giorgini, Luca Ansaloni, Niki Amadori, Carlo Coniglio, Aimone Giugni, Andrea Biscardi, Stefano Magnone, Filippo Filicori, Piergiorgio Cavallo, Silvia Villani, Francesco Cinquantini, M. Annicchiarico, Giovanni Gordini, Gregorio Tugnoli
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper has been accepted and selected for Oral Presentation in the 2010 Scientific Papers Sessions of the American College of Surgeons Annual Clinical Congress and has been presented by Dr. Salomone Di Saverio, MD in the session SP19, on Wednesday, October 6, 2010.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors
Appendix
Appendix
STROBE 2007 (v4) checklist of items to be included in reports of observational studies in epidemiologya
Section/topic | Item # | Recommendation | Reported on page # |
Title and abstract | 1 | (a) Indicate the study's design with a commonly used term in the title or the abstract | 1 |
(b) Provide in the abstract an informative and balanced summary of what was done and what was found | 2–3 | ||
Introduction | |||
Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | 4–5 |
Objectives | 3 | State specific objectives, including any pre-specified hypotheses | 4-5 |
Methods | |||
Study design | 4 | Present key elements of study design early in the paper | 5–7 |
Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | 5–7 |
Participants | 6 | (a) Cohort study—Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up | 5–7 |
Case–control study—Give the eligibility criteria, and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls | |||
Cross-sectional study—Give the eligibility criteria, and the sources and methods of selection of participants | |||
(b) Cohort study—For matched studies, give matching criteria and number of exposed and unexposed | |||
Case–control study—For matched studies, give matching criteria and the number of controls per case | |||
Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | 5–7 |
Data sources/measurement | 8a | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | 5–7 |
Bias | 9 | Describe any efforts to address potential sources of bias | 5–7 |
Study size | 10 | Explain how the study size was arrived at | 5–7 |
Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | 5–7 |
Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | 5–7 |
(b) Describe any methods used to examine subgroups and interactions | 5–7 | ||
(c) Explain how missing data were addressed | |||
(d) Cohort study—If applicable, explain how loss to follow-up was addressed | 5–7 | ||
Case–control study—If applicable, explain how matching of cases and controls was addressed | |||
Cross-sectional study—If applicable, describe analytical methods taking account of sampling strategy | |||
(e) Describe any sensitivity analyses | |||
Results | |||
Participants | 13a | (a) Report numbers of individuals at each stage of study—e.g., numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed | 7–9 |
(b) Give reasons for non-participation at each stage | |||
(c) Consider use of a flow diagram | |||
Descriptive data | 14a | (a) Give characteristics of study participants (e.g., demographic, clinical, social) and information on exposures and potential confounders | 7–9 |
(b) Indicate number of participants with missing data for each variable of interest | |||
(c) Cohort study—Summarise follow-up time (e.g., average and total amount) | 7–9 | ||
Outcome data | 15a | Cohort study—Report numbers of outcome events or summary measures over time | |
Case–control study—Report numbers in each exposure category, or summary measures of exposure | |||
Cross-sectional study—Report numbers of outcome events or summary measures | 7–9 | ||
Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g., 95 % confidence interval). Make clear which confounders were adjusted for and why they were included | 7–9 |
(b) Report category boundaries when continuous variables were categorized | 7–9 | ||
(c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | |||
Other analyses | 17 | Report other analyses done—e.g., analyses of subgroups and interactions, and sensitivity analyses | 7–9 |
Discussion | |||
Key results | 18 | Summarise key results with reference to study objectives | 9–20 |
Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | 9–20 |
Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | 9–20 |
Generalisability | 21 | Discuss the generalisability (external validity) of the study results | 9–20 |
Other information | |||
Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | 22 |
Checklist for cohort, case–control, and cross-sectional studies (combined)
Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available on the web sites of PLoS Medicine at http://www.plosmedicine.org/, Annals of Internal Medicine at http://www.annals.org/, and Epidemiology at http://www.epidem.com/). Information on the STROBE Initiative is available at www.strobe-statement.org
aGive information separately for cases and controls in case–control studies and, if applicable, for exposed and unexposed groups in cohort and cross-sectional studies
Rights and permissions
About this article
Cite this article
Di Saverio, S., Gambale, G., Coccolini, F. et al. Changes in the outcomes of severe trauma patients from 15-year experience in a Western European trauma ICU of Emilia Romagna region (1996–2010). A population cross-sectional survey study. Langenbecks Arch Surg 399, 109–126 (2014). https://doi.org/10.1007/s00423-013-1143-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1143-9